Mpox
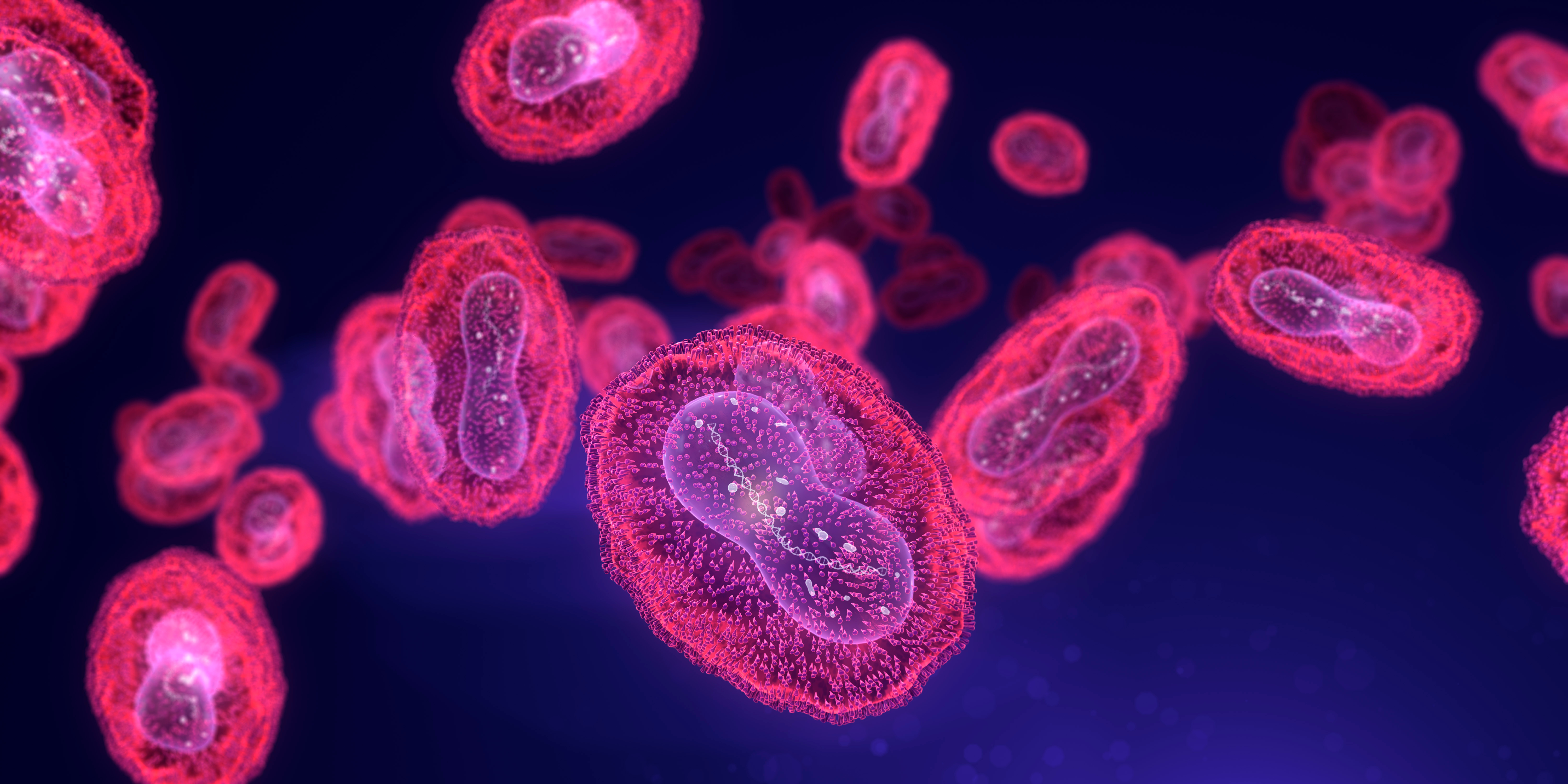
Mpox is a rare disease caused by infection with the Mpox virus. Mpox virus belongs to the Orthopoxvirus genus in the family Poxviridae. The Orthopoxvirus genus also includes variola virus (which causes smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus. Mpox is not related to chickenpox.
RUHS-Public Health Advisory: Mpox update for clinicians — clade I community spread in California; actions for Riverside County - 10/22/2025
CDPH Update: CDPH Updated Mpox Vaccination Recommendations - 9/16/2025
CDPH Health Advisory: Recent Rise of Mpox Cases in California and the Bay Area - 8/26/2025
Mpox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. Despite being named “Mpox (monkeypox)”, the source of the disease remains unknown. However, African rodents and non-human primates (like monkeys) may harbor the virus and infect people.
The first human case of Mpox was recorded in 1970. Since then, Mpox has been reported in people in several other central and western African countries. Prior to the 2022 outbreak, nearly all Mpox cases in people outside of Africa were linked to international travel to countries where the disease commonly occurs, or through imported animals.
Talk to your doctor if:
- You believe you were exposed to Mpox
OR - You develop symptoms, such as fever, headache muscle aches, swollen lymph nodes, chills exhaustion or a rash that looks like pimples or blisters
To learn more, or if you believe you have been exposed to Mpox, email mpox@ruhealth.org or call (951) 358-5107.
Frequently Asked Questions
- Where can I get vaccinated?
The JYNNEOS vaccine is available at most local health clinics, hospitals, and even at many of our mobile vaccine clinics within the community. To locate a location closest to you please visit: Upcoming Vaccine Clinics | Riverside University Health System (ruhealth.org)
Riverside County continues to work with our healthcare systems and directly communicate to eligible patients to provide details on how and where to access the JYNNEOS vaccine.
- How are vaccine doses allocated to local health jurisdictions (LHJ) in California?
California Department of Public Health allows jurisdictions to order any quantity of vials available to them up to their designated threshold. Expanded distribution contracted by the Strategic National Stockpile allows for rapid fulfilment of additional vaccine vials to as many sites as needed. Jurisdictions are confident in ordering enough vials of the vaccine to meet the need of the community.
- How can I prevent the spread of Mpox?
There are number of ways to prevent the spread of mpox, including:
- Getting vaccinated (two-doses) for MPOX. Find a vaccine near you My Turn - Manage your appointments (ca.gov).
- Continuing to reduce or avoid behaviors that increase risk for MPOX exposure until 14 days after your second dose.
- Talking to your sexual partner/s about any recent illness and being aware of new or unexplained sores or rashes on your body or your partner's body, including on the genitals and anus
- Avoiding close contact, including hugging, kissing, cuddling and sexual activity with people with symptoms like sores or rashes.
- Washing your hands often with soap and water and/or using an alcohol-based hand sanitizer
- Using appropriate PPE (like a mask, gown and gloves) when caring for people with mpox.
If you choose to remain sexually active, visit the CDPH Mpox webpage or the CDC’s Safer Sex, Social Gatherings, and Mpox webpage.
- How is the vaccine given?
The JYNNEOS vaccine is given through a shot (injection). The JYNNEOS vaccine can be given in two methods:
- The standard method is a subcutaneous injection which is a shot given beneath the skin in the upper arm. This method has been approved for people 18 years or older and is also authorized under an Emergency Use Authorization (EUA) for people under 18 years of age.
Under newer guidelines from the FDA and CDC, the vaccine can also be given through intradermal injection, in the skin layer underneath the epidermis (which is the upper skin layer) for people 18 years or older. Intradermal injection is typically given in the forearm and requires a smaller amount of vaccine than the subcutaneous injection to create a similar immune response. Intradermal injection can also be given in the upper arm or on the back below the shoulder blade.
Public health jurisdictions and healthcare providers have the flexibility to offer the intradermal or subcutaneous regimen, balancing optimal vaccine use and acceptance, feasibility of administration, and available vaccine supply. People of any age with a history of developing keloid scars, and individuals younger than 18 years of age, should receive the vaccine via the subcutaneous route. CDC recommends people get two JYNNEOS doses four weeks apart.
For more information, see the CDC’s Mpox Prevention webpage. If you have symptoms of MPOX, contact your healthcare provider. If you do not have a healthcare provider, email mpox@ruhealth.org or call (951) 358-5107 for information about getting access to a healthcare provider near you.
Information for Healthcare Professionals
- Resources for Healthcare Professionals
Riverside County
- Updated Mpox Guidance - May 31, 2023
- Assessment for Temporary Housing Form - September 22, 2022
- Supportive Home Care Guide for Mpox - July 27, 2022
- Updated Public Health Advisory - July 19, 2022
- Information For Healthcare Professionals
- CDC: Guidelines for Collecting and Handling Specimens for Mpox Testing
- Mpox Intake & Investigation Form - June 12, 2022
CDPH
CDC
- Potential for Recurrent Mpox Outbreaks Among Gay, Bisexual, and Other Men Who Have Sex with Men - United States, 2023
- CDC Report- Potential Risk for New Mpox Cases - 05/15/2023
- Mpox 2022 Cases
- Sign and Symptoms
- Clinical Recognition
- Specimen Collection
- Treatment
- Infection Control: Healthcare Settings
- Information for Laboratory Personnel
- Information for Veterinarians
- Travelers’ Health-Smallpox and Other Orthopoxvirus-Associated Infections
- Information for Healthcare Professionals
- Mpox and Smallpox Vaccine Guidance
- Monitoring People Who Have Been Exposed
- Preventing Mpox Spread in Congregate Settings
FDA
World Health Organization (WHO)
Trainings
- Mpox Lab Testing
Riverside County Testing Recommendations
Healthcare providers should test any patients with suspected Mpox. This includes any patient with a new characteristic rash or patients with risk factors for Mpox and a new rash. The rash associated with Mpox can be confused with other rashes encountered in clinical practice including herpes, syphilis, and varicella and co-infections have been reported. Providers should wear appropriate personal protective equipment (PPE) to collect specimens (see Infection Control guidance below).
Patients presenting with perianal or genital ulcers, diffuse rash, or proctitis should also be evaluated for STIs. However, the diagnosis of an STI does not exclude Mpox as a concurrent infection may be present. The clinical presentation of Mpox may be similar to some STIs, such as syphilis, herpes, lymphogranuloma venereum (LGV), or other etiologies of proctitis.
Commercial testing is available
Commercial testing for Mpox continues to expand. Testing is now available through Quest Diagnostics, LabCorp, Aegis Sciences and Mayo Clinic Laboratories. LabCorp, Mayo Clinic Laboratories, and Aegis Sciences are using the CDC’s orthopoxvirus test (which detects all non-smallpox related orthopoxviruses, including Mpox). The Quest assay is real time PCR test developed by Quest that detects DNA of non-variola orthopoxviruses and Mpox virus (West African clade)—see Quest FAQs. CDC anticipates additional commercial laboratories will come online this month.
Providers should submit specimens through commercial labs if possible. Follow specimen collection instructions provided by the laboratory. Public health approval is not required to submit specimens to a commercial lab, however providers should notify public health about patients suspected to have Mpox without waiting for results to return to allow for contact tracing efforts to begin expeditiously.
Providers using commercial labs must report all Riverside County residents with orthopoxvirus positive and/or presumptive positive test results (see Reporting).
Public Health Laboratory
Providers that do not have access to commercial orthopoxvirus testing, may request testing for suspected cases by submitting a Mpox intake form and photos of the rash/lesions via secure email to bcole@ruhealth.org
Testing Guidance
If a patient is evaluated and Mpox is high on the differential diagnosis, collect two swabs from two different lesions for preliminary and confirmatory testing as follows:
- Vigorously swab or brush lesion with two separate sterile dry polyester or Dacron swabs. (two from each lesion)
- Break off end of applicator of each swab into a sterile 1.5- or 2-mL screw-capped tube with O- ring or place 2 entire swabs in 2 separate sterile containers. Do not add or store in viral or universal transport media.
- The two separate sterile containers should be placed in 2 separate biohazard bags and refrigerated at 4C.
Specimens being tested through Public Health, will be picked by a RUHS courier, within 24 hours Monday through Friday. Store specimens at -80C if it is greater than 72 hours between specimen collection and pickup.
Swabs can be collected and stored at the proper temperature without waiting to discuss the case with Public Health. This will avoid outpatients needing to be recalled should they meet criteria for testing through Public Health.
Infection Control
Patients presenting with suspected Mpox should be placed, as soon as possible, into a single person exam room with door closed, or an airborne infection isolation room, if available. The patient should remain masked, as tolerated (as currently required for all persons in healthcare settings) and any exposed skin lesions should be covered with a sheet or gown.
Healthcare personnel (HCP) evaluating patients with suspected Mpox should wear the following personal protective equipment (PPE): gloves, gown, eye protection (goggles or face shield) and a N95 or equivalent or higher-level respirator. HCP should don PPE before entering the patient’s room and use for all patient contact. HCP should remove and discard gloves, gown, and eye protection, and perform hand hygiene prior to leaving the patient’s room; the N95 respirator should be removed, discarded, and replaced with a mask for source control after leaving the patient’s room and closing the door.
Any EPA-registered hospital-grade disinfectant should be used for cleaning and disinfecting environmental surfaces.
All disposable equipment used for obtaining swabs (e.g., scalpel) must be properly discarded according to the facility’s established procedures.
CDPH
- For local health departments
- Healthcare Provider Mpox Health Advisory, May 27, 2022: Mpox Virus Infection in the United States and Other Non-endemic Countries
CDC
- Mpox For Providers
- Mpox Sexual Health

Mpox guidance for people who are sexually active.