PREVENTION
What is Prevention?
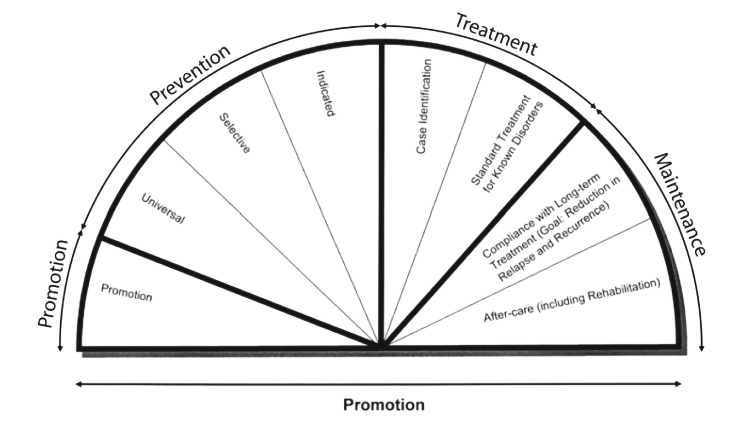
Prevention in health is often defined as actions that help to "keep people healthy and well" by reducing the risk of poor health, illness, injury, and death (Australian Prevention Partnership, 2023). The National Institutes of Health classifies prevention into three distinct levels: universal, selective, and indicated.
Universal prevention strategies are inclusive of the entire population, as they intend to provide some benefit or reduce the risk of poor health outcomes. Selective prevention strategies focus on populations with an "elevated risk" whereas indicated prevention strategies require more "intensive interventions" but are still not considered treatment (National Research Council and Institute of Medicine, 2009).
THEORIES OF BEHAVIORAL CHANGE
Theories of behavior change provide context on factors that influence health behaviors and can help identify interventions to address root causes of poor health outcomes. While this list is not exhaustive, two notable theories of behavior change are included to guide school districts when selecting substance use prevention strategies.
HEALTH BELIEF MODEL
The Health Belief Model (HBM) was developed to understand why people do not adopt disease prevention strategies or engage in screening tests for early detection of disease. HBM suggests that "a person’s belief in a personal threat of an illness or disease together with a person’s belief in the effectiveness of the recommended health behavior or action will predict the likelihood the person will adopt the behavior" (Boston University, 2022, para 1.).
The foundations of HBM explain that health behaviors are based on the following:
- The desire to avoid illness or disease.
- The belief that a specific health action will prevent, or cure, illness or disease.
- The actions one takes depends on their perceptions of the benefits and barriers of the action.
Source: Boston University, 2022
HEALTH BELIEF MODEL - SIX CONSTRUCTS
A total of six constructs are included:
"PERCEIVED SUSCEPTIBILITY
This refers to a person’s subjective perception of the risk of acquiring an illness or disease. There is wide variation in a person’s feelings of personal vulnerability to an illness or disease.
PERCEIVED SEVERITY
This refers to a person’s feelings on the seriousness of contracting an illness or disease (or leaving the illness or disease untreated). There is wide variation in a person’s feelings of severity, and often a person considers the medical consequences (e.g., death, disability) and social consequences (e.g., family life, social relationships) when evaluating the severity.
CUE TO ACTION
This is the stimulus needed to trigger the decision-making process to accept a recommended health action. These cues can be internal (e.g., chest pains, wheezing, etc.) or external (e.g., advice from others, illness of family member, newspaper article, etc.).
PERCEIVED BARRIERS
This refers to a person’s feelings on the obstacles to performing a recommended health action. There is wide variation in a person’s feelings of barriers, or impediments, which lead to a cost/benefit analysis. The person weighs the effectiveness of the actions against the perceptions that it may be expensive, dangerous (e.g., side effects), unpleasant (e.g., painful), time-consuming, or inconvenient
PERCEIVED BENEFITS
This refers to a person’s perception of the effectiveness of various actions available to reduce the threat of illness or disease (or to cure illness or disease). The course of action a person takes in preventing (or curing) illness or disease relies on consideration and evaluation of both perceived susceptibility and perceived benefit, such that the person would accept the recommended health action if it was perceived as beneficial.
SELF-EFFICACY
This refers to the level of a person’s confidence in his or her ability to successfully perform a behavior. This construct was added to the model most recently in mid-1980. Self-efficacy is a construct in many behavioral theories as it directly relates to whether a person performs the desired behavior" (Boston University, 2022, para 3.)
Source: Boston University, 2022
STAGES OF CHANGE THEORY
The Transtheoretical Model (Stage of Change) was developed based off smoking cessation research. Stages of Change provides detail on the steps of decisionmaking, acknowledging that people do not change quickly, but happens continuously through a cyclical process. Stages of Change is a model and other behavior change theories can be applied to the different stages.
STAGES OF CHANGE THEORY - SIX CONSTRUCTS
A total of six constructs are included:
"PRECONTEMPLATION
In this stage, people do not intend to take action in the foreseeable future (defined as within the next 6 months). People are often unaware that their behavior is problematic or produces negative consequences. People in this stage often underestimate the pros of changing behavior and place too much emphasis on the cons of changing behavior.
CONTEMPLATION
In this stage, people are intending to start the healthy behavior in the foreseeable future (defined as within the next 6 months). People recognize that their behavior may be problematic, and a more thoughtful and practical consideration of the pros and cons of changing the behavior takes place, with equal emphasis placed on both. Even with this recognition, people may still feel ambivalent toward changing their behavior.
PREPARATION (DETERMINATION)
In this stage, people are ready to take action within the next 30 days. People start to take small steps toward the behavior change, and they believe changing their behavior can lead to a healthier life.
ACTION
In this stage, people have recently changed their behavior (defined as within the last 6 months) and intend to keep moving forward with that behavior change. People may exhibit this by modifying their problem behavior or acquiring new healthy behaviors.
MAINTENANCE
In this stage, people have sustained their behavior change for a while (defined as more than 6 months) and intend to maintain the behavior change going forward. People in this stage work to prevent relapse to earlier stages.
TERMINATION
In this stage, people have no desire to return to their unhealthy behaviors and are sure they will not relapse. Since this is rarely reached, and people tend to stay in the maintenance stage, this stage is often not considered in health promotion programs" (Boston University, 2022).
Source: Boston University, 2022